A cancer misdiagnosis can be devastating, not only for patients whose lives may be irreversibly impacted, but also for physicians facing resulting lawsuits. These claims often result in significant legal, financial, and emotional consequences for healthcare providers, making them especially impactful.
Physicians need to know whether misdiagnosis errors—especially those involving delayed cancer diagnoses—are covered by medical malpractice insurance.
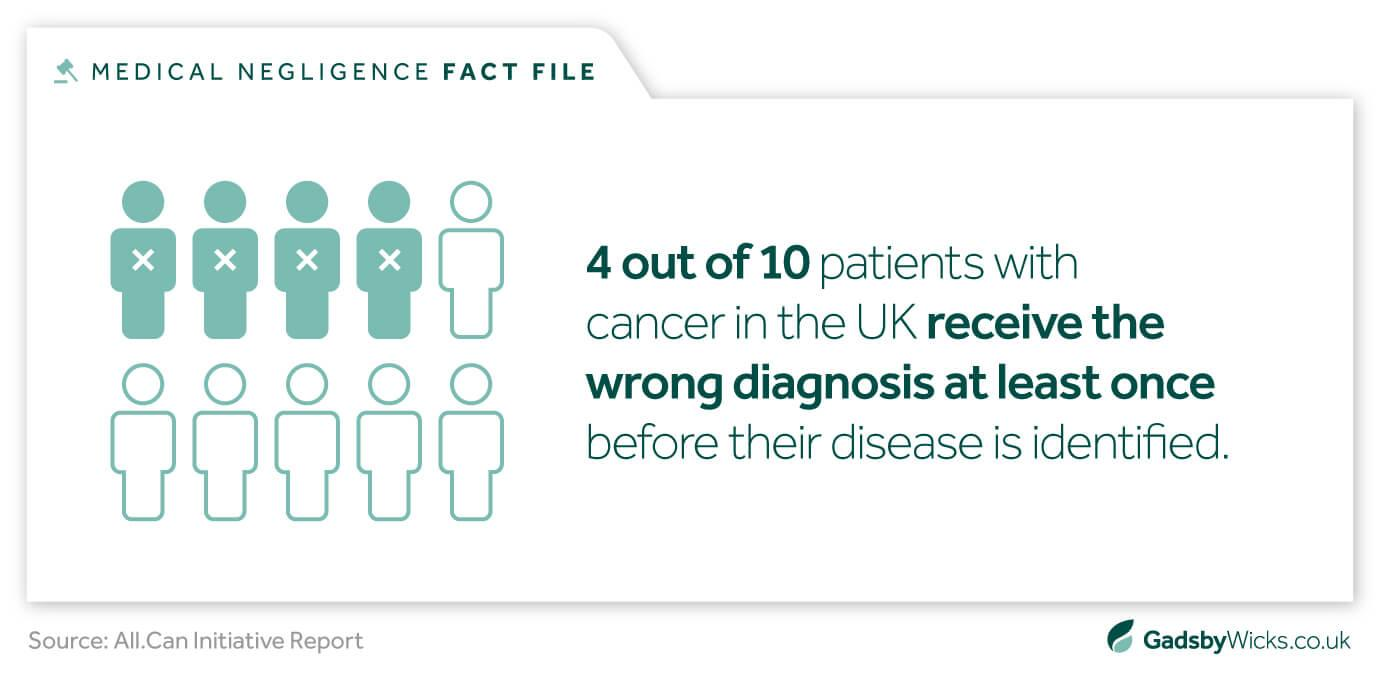
According to a study published in BMJ Quality & Safety, diagnostic errors affect approximately 12 million adults in the U.S. each year, with cancer among the top three most commonly misdiagnosed conditions. This underscores how widespread the issue is—and why both patients and physicians need to understand its consequences and coverage.
![]()
Why Cancer Misdiagnosis Happens: The Role of Medical Negligence?
There are several causes of cancer misdiagnosis, which can primarily be grouped into human errors and system-level mistakes. Nonetheless, the error can be categorized as medical negligence if it results from a departure from the recognized standard of care. Typical reasons include:
1. Failure to Order Appropriate Tests
Physicians may dismiss early symptoms or rely solely on basic diagnostic tools, overlooking the need for more definitive tests like biopsies, MRIs, or CT scans.
For example, a patient reporting persistent abdominal pain might experience a delayed colorectal cancer diagnosis if not referred for a colonoscopy.
2. Improper Interpretation of Diagnostic Results
Imaging scans or tissue samples can be misread by radiologists or pathologists, resulting in either a false negative, missing the cancer entirely, or a false positive—diagnosing cancer when there is none.
These errors can delay treatment and may also lead to aggressive or unnecessary interventions.
3. Lack of Follow-Up on Abnormal Test Findings
Even when initial tests raise red flags, communication breakdowns or administrators overlooking them can prevent timely follow-up.
For example, after a flagged mammogram, no biopsy or follow-up imaging may be scheduled. Therefore, cancer may go undetected for months or even years.
4. Poor Communication Between Medical Professionals
Miscommunication or lack of coordination among primary care physicians, specialists, radiologists, and laboratory staff can result in critical information being overlooked.
A test result might not be acted upon if it is not clearly communicated during a patient handoff.
5. Inadequate Patient Evaluation or Referral Delays
Some misdiagnoses stem from rushed consultations or failure to conduct a thorough patient history and physical examination. In other situations, a general practitioner can be reluctant to promptly refer a patient to a specialist, which could lead to missed opportunities for early intervention.
These errors may result in a delayed cancer diagnosis, which may limit available treatments, cause the disease to worsen, or even cause death.
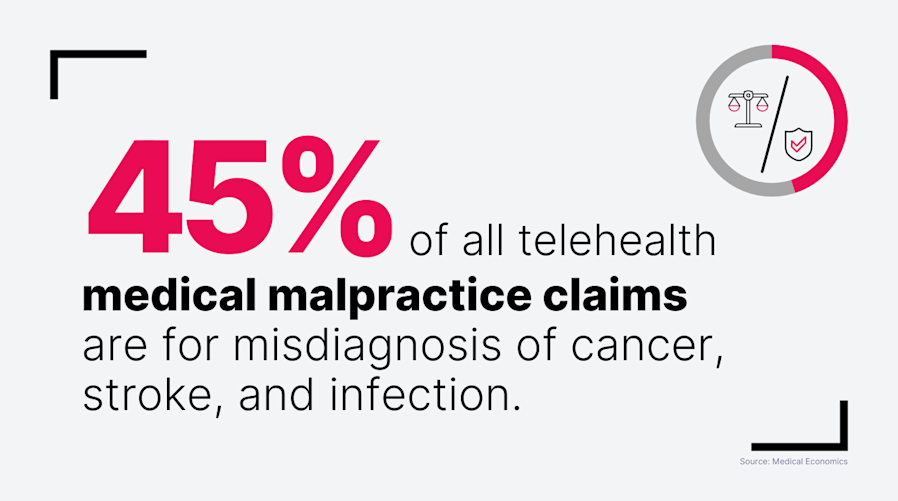
The Role of Telehealth in Cancer Misdiagnosis
While telehealth offers greater accessibility, it also introduces new risks for misdiagnosis. Limited physical examinations, reduced access to real-time diagnostics, and fragmented care can all contribute to missed or delayed cancer diagnoses.
Physicians relying on virtual care must be extra cautious in patient evaluation and follow-up, ensuring that any concerning symptoms trigger in-person visits or appropriate testing.
Commonly Misdiagnosed Cancers
There are some cancers that are more commonly misdiagnosed because of mild or overlapping symptoms. Some of the most often mistaken cancers include:
- Breast Cancer – Can be overlooked in dense breast tissue or due to misinterpreted mammograms.
- Lung Cancer – Symptoms such as cough and fatigue are often mistaken for a less serious condition.
- Colorectal Cancer – Easily mistaken for IBS or hemorrhoids.
- Pancreatic Cancer – Early symptoms often go unnoticed, as they are nonspecific and frequently misunderstood.
- Lymphoma – Common symptoms like swollen lymph nodes are often attributed to infection.
These cancers are particularly associated with delayed diagnosis malpractice claims due to their aggressive progression when left untreated.
When Does a Cancer Misdiagnosis Become Medical Malpractice?
Not all instances of cancer misdiagnosis become medical malpractice. To meet the legal definition of malpractice, a few elements are usually necessary:
- A doctor-patient relationship existed
- The provider deviated from the accepted standard of care
- The misdiagnosis led to harm that would have been avoidable
- The harm resulted in measurable damages (financial, physical, and emotional)
For example, if a doctor neglected to order a biopsy for an unusual lump and thus delayed the cancer diagnosis for months as it goes into stage progression, this could constitute medical malpractice resulting from misdiagnosis.
What Damages Are Available in a Cancer Misdiagnosis Case?
The damages awarded in cancer misdiagnosis suits can be considerable—the longer the delay, the worse the prognosis. A patient can recover:
- Economic Damages: Medical bills, lost income, future treatment costs
- Non-Economic Damages: Pain and suffering, loss of quality of life, emotional distress
- Punitive Damages: In rare cases of gross negligence or willful misconduct
For a physician, this means that a medical malpractice policy providing not only for litigation defense but with limits adequately high to pay large damages if they occur is necessary.
Legal Consequences for Physicians in a Cancer Misdiagnosis Lawsuit
![]()
Physicians can have significant personal and professional consequences from a lawsuit alleging a cancer misdiagnosis. These cases can result in serious legal and financial consequences:
Reputation Damage
Even an unfounded allegation can lead to a breach of patient trust, cause damage to professional relationships, and lead to loss of referrals, diminished credibility, and reduced respect for one’s practice.
License Review
Serious or repeated misdiagnoses can be investigated by the state medical boards, which can lead to suspension, additional coursework, or even some level of disciplinary action.
Increased Insurance Premiums
Following a claim, providers often face significantly higher malpractice insurance premiums—or, in some cases, difficulty renewing coverage altogether.
Emotional Toll
A doctor and their staff may suffer burnout, anxiety, or a disrupted clinic environment due to the emotional and operational strain of litigation.
For this reason, having full medical malpractice insurance coverage is crucial. It helps guard against malpractice claims involving delayed cancer diagnosis and gives doctors the emotional and legal support they need to handle the procedure with assurance.
Does Medical Malpractice Insurance Cover Cancer Misdiagnosis?
In general, medical malpractice insurance does cover misdiagnosis of cancer. The terms of the coverage, however, will be determined by the details of the medical malpractice policy. Because cancer misdiagnosis claims are so serious, it’s critical to understand the specifics of your insurance.
A misdiagnosis where cancer is either missed, incorrectly diagnosed, or diagnosed too late can create significant exposure and liability, whether it’s in the form of large settlement payouts or jury-verdict settlements. Here are items health care professionals should examine when reviewing their medical malpractice insurance coverage:
1. Policy Type: Claims-Made vs. Occurrence-Based
Understanding your policy structure is the first step:
Claims-made policies only provide coverage if the claim is filed while the policy is active. If a cancer misdiagnosis occurred during coverage but the lawsuit is filed after the policy expires, you may not be covered—unless you purchase tail coverage.
Occurrence-based policies, on the other hand, cover occurrences that have happened during the policy while it was active, no matter when the lawsuit is filed thereafter. Occurrence-based policies generally provide broader long-term protection; however, they usually have higher premiums.
Given that delayed cancer diagnosis malpractice claims can arise months or even years after the misdiagnosis, this distinction is crucial.
To understand which policy better suits your long-term needs, explore this detailed breakdown on Claims-Made vs. Occurrence Malpractice Insurance.
2. Exclusions and Limitations
Policies for medical malpractice insurance are not all made equal. Some might include exclusions for specific high-risk treatment types, diagnostic services, or specialties that are more likely to be sued, such as radiology or oncology.
Common exclusions to watch for:
- Serious carelessness or deliberate wrongdoing
- Certain types of cancer treatment protocols
- Claims arising from care provided outside approved settings or jurisdictions
Always review your policy language carefully—or work with a broker—to ensure there are no gaps that could leave you vulnerable in a cancer misdiagnosis lawsuit.
3. Tail Coverage (Extended Reporting Period Coverage)
Because cancer misdiagnosis claims are often filed long after the actual medical encounter, physicians who leave a practice or switch insurers should strongly consider purchasing tail coverage. This add-on extends your protection even after the original claims-made policy expires.
If a former patient presses a claim against you after you leave, you’re still covered, which underscores why tail coverage is essential. This is especially important in higher-risk professions like radiology, primary care, and oncology.
4. Adequate Coverage Limits
An incorrect cancer diagnosis could result in severe financial consequences, ranging from hundreds of thousands to even millions of dollars. Settlements or verdicts involving malpractice lawsuits—especially those involving serious complications, wrongful death, or advanced-stage cancer—can reach hundreds of thousands or even millions.
Make sure your policy includes:
- Sufficient per-claim and aggregate limits
- Legal defense coverage (which should be outside policy limits if possible)
- Optional supplemental coverages for reputational damage or administrative defense
Inadequate limits could mean you’re personally responsible for any amounts above what your insurance covers—an enormous risk in cancer-related cases.
Why This Matters
The reality is simple: cancer misdiagnosis lawsuits are among the most emotionally charged and legally complex types of malpractice claims. Patients may face worsened prognoses, more aggressive treatment regimens, or even death due to delays or errors in diagnosis. That makes these cases not only high-risk but often high-payout.
![]()
Without the right medical malpractice insurance coverage, healthcare providers risk both financial ruin and career disruption.
Ensuring your policy explicitly covers cancer misdiagnosis, includes sufficient limits, and offers a flexible coverage structure—these are among the most important risk management steps a healthcare provider can take.
In an increasingly complex healthcare landscape, staying informed about the legal and insurance implications of diagnostic errors isn’t optional—it’s essential. Physicians must ensure their malpractice insurance policies offer sufficient protection, especially against the high stakes of cancer misdiagnosis claims. When in doubt, consult a trusted insurance advisor or legal expert.