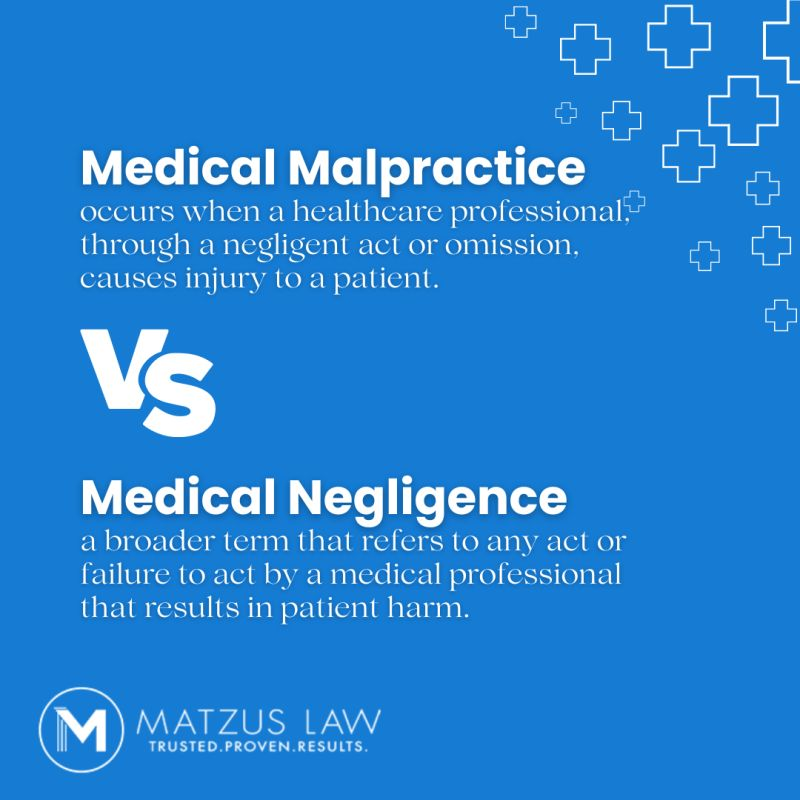
When something goes wrong during a medical procedure or treatment, it can leave patients and their families feeling blindsided. You might be asking: “Was this a simple mistake—or was it something more serious?” In these situations, you’ll often hear two terms come up: medical negligence and medical malpractice.
At first glance, they might sound like the same thing. Both involve errors in healthcare, both can result in serious harm, and both may lead to legal consequences. But in reality, there’s an important difference—and knowing that distinction could help you understand your rights, what went wrong, and what steps to take next.
What Is Medical Negligence?
Medical negligence is more common—and often less understood—than medical malpractice.
Medical negligence happens when a medical provider fails to do something they should do or does something they shouldn’t do, which results in accidental damage. Again, this is not about intentional wrongdoing or deliberate errors. Most negligence cases involve inattention, distraction, or failure to follow protocols.
Real-World Examples of Medical Negligence:
- A nurse forgets to administer a scheduled dose of medication.
- A doctor prescribes a new drug without reviewing a patient’s allergy history.
- A lab technician mislabels a blood sample, leading to a delayed diagnosis.
- Outdated or improperly cleaned equipment is used during a procedure.
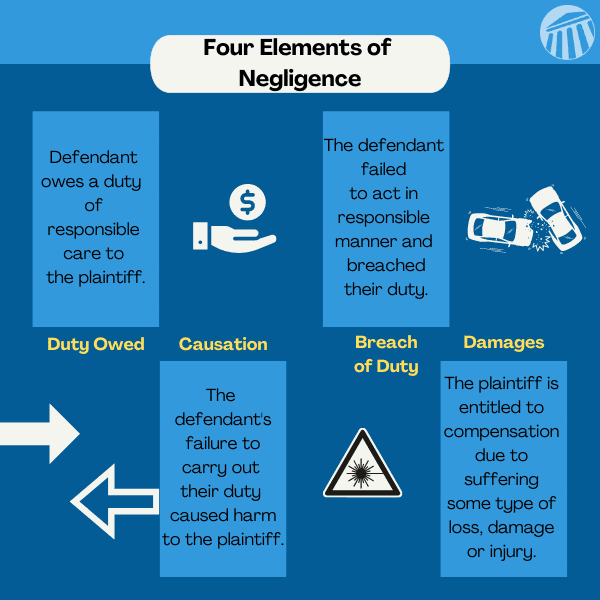
In each of these cases, the healthcare providers didn’t mean to cause harm—but their actions, or lack of action, led to it. It’s a breach of the duty of care that any competent professional would be expected to uphold, and these mistakes are more common than we think.
What Is Medical Malpractice?
Now, let’s examine medical malpractice. This is where things are elevated to a different level, not just legally but also ethically and professionally.
Medical malpractice occurs when a healthcare provider does not merely make an error; the healthcare provider intentionally disavows or violates established standards of care and is clearly incompetent or reckless. It is not just neglect; it is professional misconduct.
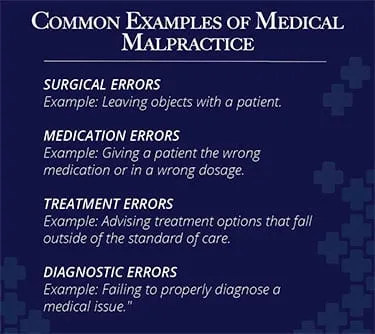
Real-World Examples of Medical Malpractice:
- A surgeon performs a procedure on the wrong body part even after reviewing the surgical chart.
- A doctor sees abnormal test results but dismisses them and sends the patient home.
- A radiologist misreads a scan due to inattention, not because the image was unclear.
- A physician fails to obtain informed consent before a high-risk surgery.
One of the most widely discussed malpractice cases in recent years involved a woman in New Jersey who underwent spinal surgery only to discover it was performed at the wrong site. The end result? A jury awarded her $77 million. This was not a technical error; it was a willful disregard for critical surgical protocols.
Malpractice cases often draw more attention because they involve a gross deviation from expected standards, and the harm caused is usually severe. That’s why malpractice is considered a type of negligence, but one with far greater legal weight.
Understanding Where Things Go Wrong
Let’s start with medical negligence, because it’s often where things begin. Negligence is when a healthcare professional fails to provide the expected standard of care, and that failure unintentionally causes harm.
For example, say a nurse is overworked and skips a routine post-op check—not realizing the patient is showing early signs of internal bleeding. The oversight wasn’t intentional, but the consequences were serious. That’s medical negligence. It wasn’t an act of malice, but rather a failure to act when necessary.
Unfortunately, this isn’t rare. A Johns Hopkins study estimated that medical errors are the third leading cause of death in the U.S., with more than 250,000 deaths each year. Many of these are tied to simple, preventable mistakes—missed symptoms, wrong medications, communication failures. They’re not always dramatic, but they are life-changing.
Now, take that one step further. If a doctor had access to your full test results, saw signs of a serious condition, but chose to ignore them or rushed to a diagnosis without considering those red flags—that’s no longer just negligence. That’s medical malpractice.
So, What’s the Difference Between Negligence and Malpractice?
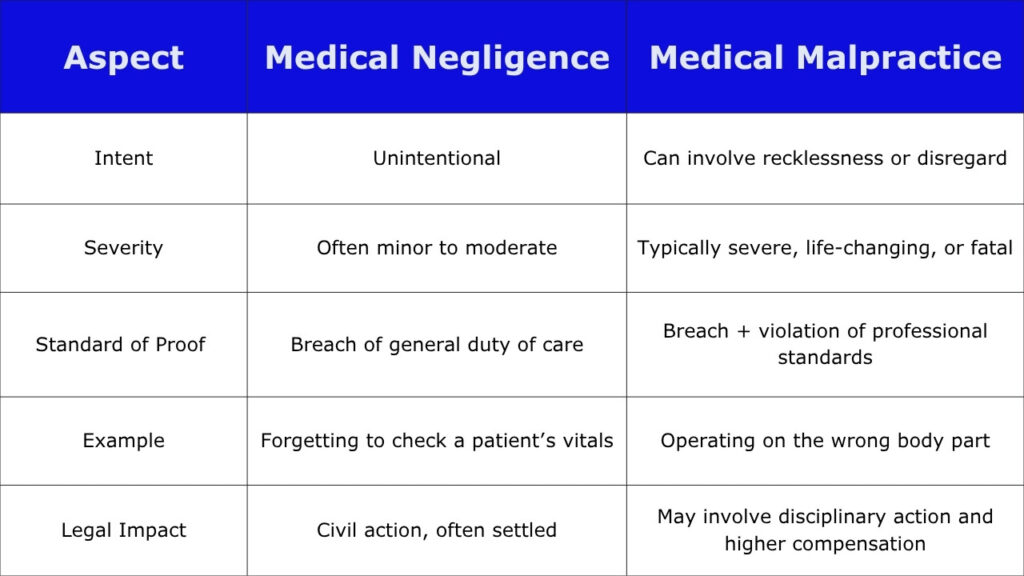
At their core, both negligence and malpractice involve a breach of duty and harm to the patient. The key difference lies in the intent and behavior of the medical professional.
The Legal Angle: Why It Matters
So why does this distinction matter? Legally, a medical malpractice case is more difficult to prove than a negligence case. It’s not just about proving that something went wrong; you must also show the provider violated medical standards that a competent professional would have followed under similar circumstances.
This is why medical malpractice cases usually require expert witnesses, reviews of the medical records, and, in some cases, months or years of investigation.
When you prove a negligence case, you still have to show that there was a breach of the duty of care and that there was harm, but you don’t need to prove intent or gross misconduct.
Aside from the legal process, the emotional toll on a patient is often the same: lost time, long recovery times, expensive treatment, and, in some cases, irreversible damage.
Consequences of Negligence in Healthcare
The consequences of negligence in healthcare can be as devastating as those from malpractice—physically, emotionally, and financially.
For Patients:
- Delayed recovery or worsened condition
- Permanent disability
- Emotional distress, PTSD, or loss of trust in the medical system
- Financial burdens due to additional treatments or lost wages
For Providers and Hospitals:
- Legal action and monetary settlements
- Damage to professional reputation
- Regulatory penalties or license suspension
- Changes in policies or loss of accreditation
Real-World Impact:
Hospitals can be required to change safety protocols after attention-grabbing negligence incidents in health care, and doctors can get temporary and permanent bans from practicing medicine.

Can Patients Protect Themselves?
Absolutely – while it may not be possible to avoid every mistake, you can minimize your risks.
- Avoid misunderstandings about your care—ask questions about your medications, diagnosis, or any procedures before accepting their recommendations.
- Bring somebody along with you to appointments. A second person can help ensure you understand your condition and catch anything you might miss during the appointment. They can also help identify if something seems off—especially when unusual situations arise.
- Verify the instructions and timelines of follow-up visits.
- Create a record of all tests, results, and any contact with healthcare professionals involved in the patient’s care.
- Speak up if anything feels wrong — it’s your health!
If something still goes wrong, it’s crucial to consult a legal professional who understands the intricacies of medical malpractice cases and negligence cases in healthcare.
Understanding the difference between medical malpractice and medical negligence isn’t just legal jargon—it’s about protecting yourself and your loved ones from preventable harm. Both involve breakdowns in care, but the degree, intent, and legal path can vary drastically.
If a healthcare provider has harmed you, consult a legal expert to assess whether your situation involves negligence in healthcare or escalates to medical malpractice. The sooner you act, the more options you may have for justice and compensation.
Here are answers to some frequently asked questions about negligence and malpractice.