Walking into an emergency room (ER) can feel like stepping into a whirlwind, where every second counts and decisions are made under intense pressure. With more than 130 million visits to U.S. ERs annually, the high-stakes environment naturally increases the likelihood of mistakes.
While ER teams often achieve remarkable outcomes, the fast pace and complexity of care make errors more likely. These mistakes can range from misdiagnoses to procedural oversights and in some cases, they result in serious harm or medical malpractice claims
Understanding the most common emergency room errors can help patients stay informed and empower healthcare providers to enhance safety and reduce risks.
1. Misdiagnosis or Delayed Diagnosis
Misdiagnosis or delayed diagnosis is one of the most common and serious ER mistakes. About 5.7% of U.S. emergency visits involve a misdiagnosis, and nearly 65% of ER malpractice claims stem from diagnostic errors, often resulting in serious harm or death.
These errors usually happen when serious conditions mimic minor ones, for example, a heart attack mistaken for indigestion or a stroke overlooked during triage. Delays in diagnosis can prevent timely treatment, leading to permanent injury or even death, making this a major cause of medical malpractice claims.
2. Medication Errors
Medication errors occur when the wrong drug, dosage, or treatment is given, or when drug interactions or allergies are overlooked. These mistakes can lead to overdoses, adverse reactions, or untreated conditions.
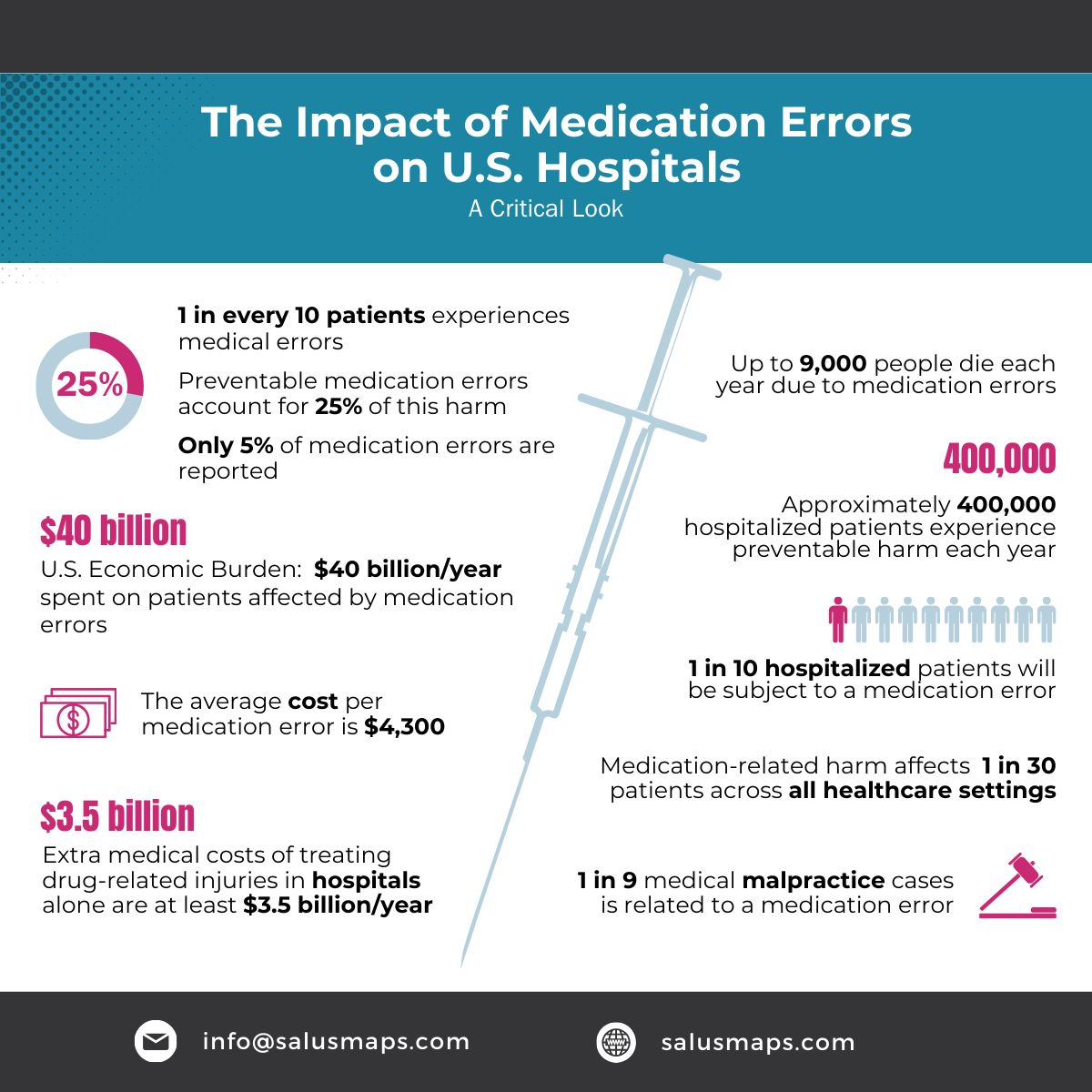
Although preventable through proper checks and communication, medication errors remain a top cause of ER malpractice claims, often resulting in extended hospital stays, lasting injuries, or even death.
3. Improper Performance of Procedures
In an emergency room, procedures often need to be performed quickly, whether it’s stitching a deep wound, setting a fracture, inserting an IV line, or conducting an urgent surgery. But in the rush to act, errors in technique or judgment can occur. These mistakes may include wrong-site surgeries, poorly executed stitches, mishandled intubations, or improper use of medical devices.
The problem is that even seemingly minor errors can have lasting consequences. A botched suture could lead to infection and scarring, while an improperly placed breathing tube can cause brain damage due to a lack of oxygen. In more complex situations, a mistake in surgery could result in permanent disability or even death.
Part of the challenge is that not every provider in the ER has the same level of experience with every emergency procedure. Combine that with fatigue, stress, and overcrowding, and the likelihood of errors increases. For patients and families, these procedural mistakes can turn a moment of trust into a devastating ordeal, one that frequently becomes the basis for medical malpractice insurance claims.
4. Delayed Treatment
Delayed treatment is one of the most critical errors in emergency rooms, where time often determines life or death. When patients with severe conditions such as heart attacks, strokes, or traumatic injuries do not receive timely interventions, the chances of recovery drastically decline.
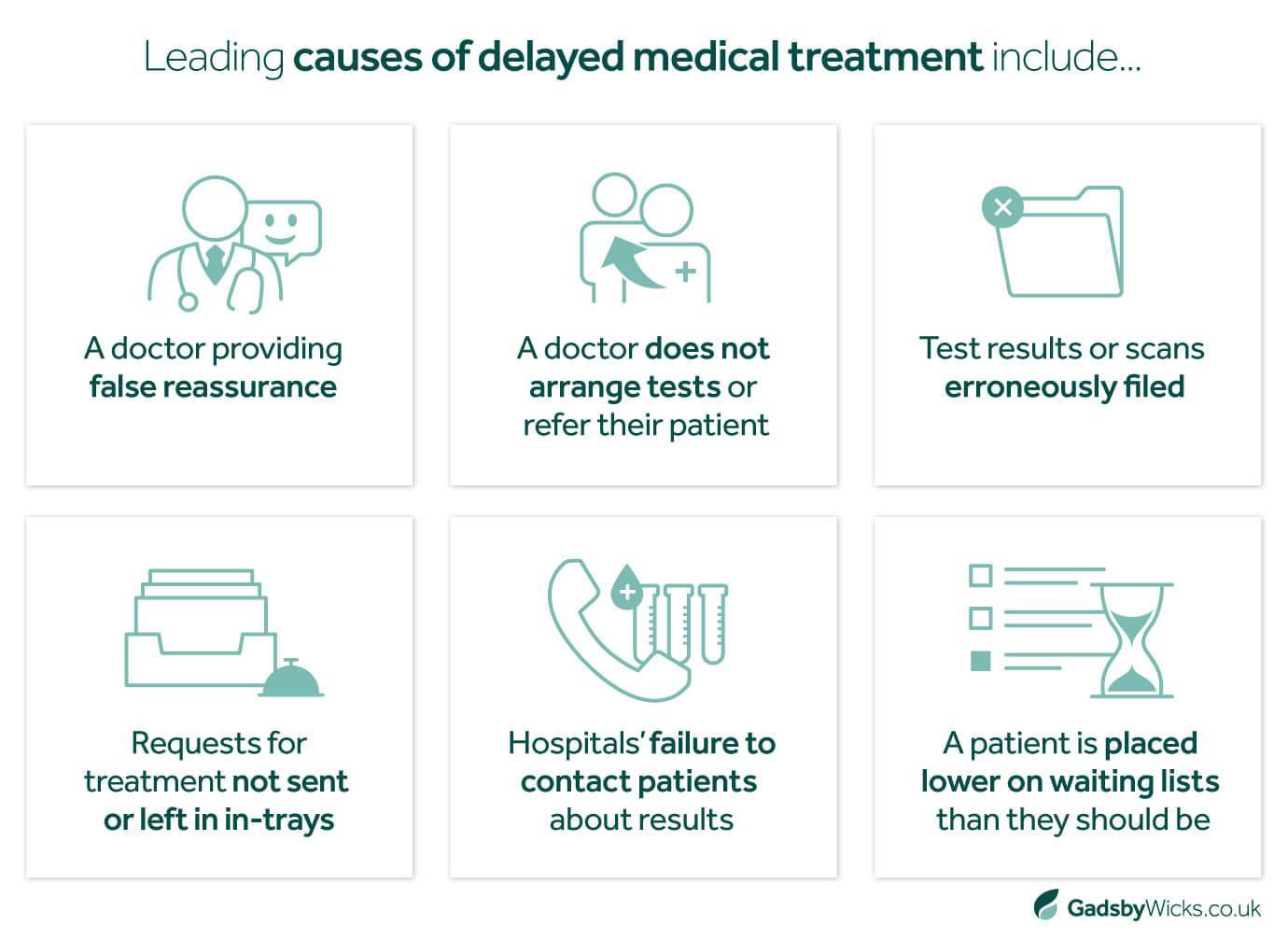
Overcrowded ERs, understaffing, or mismanagement of resources can all contribute to these harmful delays. Even something as seemingly simple as a misstep in the triage process can push urgent cases further down the line, resulting in irreversible complications or fatalities.
From a legal standpoint, delayed treatment leaves healthcare providers and facilities particularly vulnerable to malpractice claims.
Families often argue that the harm or death could have been avoided had care been rendered promptly. Beyond medical malpractice lawsuits, the ethical responsibility of healthcare professionals makes avoiding delays imperative. Implementing efficient triage systems, ensuring adequate staffing, and leveraging technology for faster decision-making are some of the key ways to reduce the risk of treatment delays in emergency settings.
5. Lab and Test Result Errors
Lab and test result errors are a significant but often overlooked source of mistakes in emergency care. Even when tests are performed, problems like lost results, transcription errors, or misinterpretations can derail diagnosis and treatment. For instance, a mislabeled blood sample or a delayed lab report can lead to misdiagnosis or inappropriate interventions, putting the patient’s health at serious risk.
These errors also create communication challenges among medical staff. Delays or mistakes in sharing results can disrupt care plans and reduce patient trust. Often, these issues stem from inadequate tracking systems, human oversight, or the fast-paced ER environment.
Implementing double-check procedures, better electronic medical records, and clear lab-to-provider communication can help reduce these errors and improve patient safety.
6. Imperfect Discharges
Discharging a patient too early is a common emergency room error. Often, ERs face bed shortages or high patient volumes, which can pressure staff to release patients before their conditions are fully evaluated. This may mean sending someone home while serious issues, like internal bleeding or infections, remain undetected.
Improper discharges are a frequent cause of medical malpractice claims, especially when patients experience worsening symptoms or complications after leaving the hospital. Ensuring proper follow-up, clear instructions, and thorough evaluation before discharge can significantly reduce these risks and improve patient safety.
7. Communication Breakdowns
Clear communication and teamwork are critical in the fast-paced environment of an ER. When important information such as allergies, test results, or patient history is not shared accurately, mistakes can quickly escalate. Shift changes, overlapping responsibilities, and hurried handoffs often make these errors more likely.
Experts note that communication failures are a leading cause of preventable harm in emergency rooms. Ensuring structured handoffs, double-checking critical information, and fostering a culture of open communication can help reduce mistakes and improve patient outcomes.
![]()
8. Failure to Follow Up
After a patient leaves the ER, proper follow-up care is crucial to ensure recovery. Missing steps like reviewing lab results, monitoring for complications, or scheduling post-treatment check-ins can allow serious issues to go unnoticed.
Omitting follow-up care is a common reason for medical malpractice claims, especially when a patient’s condition worsens unexpectedly. Clear instructions, scheduled check-ins, and diligent review of test results can help prevent complications and protect both patients and healthcare providers.
9. Systemic Failures & Burnout
Not all emergency room errors are due to individual mistakes; many stem from systemic issues. Understaffing, inadequate training, and overwork create an environment where even the most skilled providers are more likely to make errors.
Burnout among ER staff further increases the risk of mistakes, from missed symptoms to delayed treatments. Strengthening staffing levels, providing ongoing training, and addressing workplace stress are essential steps to reduce errors and improve patient safety.
10. Documentation and Triage Errors
Accurate triage and documentation are critical in the ER, where prioritizing patients correctly can save lives. Misclassifying a serious condition, like labeling a pulmonary embolism as low-risk, can delay urgent care and put the patient in danger.
Incomplete or inaccurate documentation compounds these risks by creating confusion among staff, delaying treatments, and increasing the likelihood of errors. Implementing clear triage protocols and thorough record-keeping can help prevent these mistakes and improve overall patient safety.
11. Defensive Medicine Gone Awry
The fear of lawsuits sometimes leads ER providers to practice defensive medicine, ordering excessive tests or avoiding high-risk patients to protect themselves legally. While the intention is to prevent mistakes, these actions can have unintended consequences.
Over-testing increases healthcare costs, exposes patients to unnecessary procedures, and can even delay the right treatment. Despite these efforts, defensive medicine does not fully eliminate the risk of medical malpractice claims. Striking a balance between caution and effective care is key to ensuring patient safety while reducing unnecessary interventions.
These errors not only create malpractice exposure but also increase costs for providers and facilities. See how medical errors can influence insurance premiums. Understanding this connection highlights why reducing emergency room errors is not only critical for patient safety but also for controlling insurance premiums, helping to build a stronger system that supports both healthcare workers and patients.
Why These Errors Lead to Malpractice Claims
In the U.S., to succeed in a medical malpractice claim, the plaintiff must show:
- A duty of care existed.
- That duty was breached (i.e., there were errors in treatment).
- The breach caused harm that led to damages.
Diagnostic mistakes, procedural errors, and communication breakdowns are especially potent grounds for a claim because they directly affect outcomes and often represent a clear deviation from the standard of care.
Making It Personal And Preventable
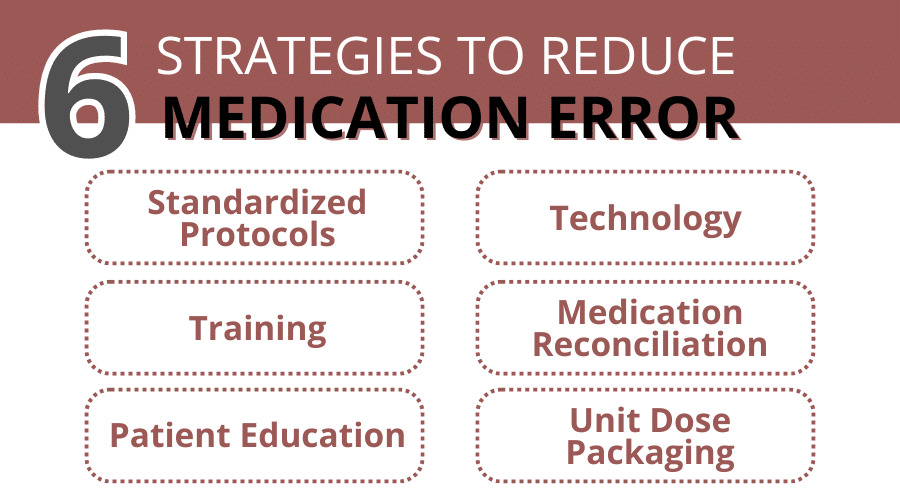
ER errors can feel clinical and abstract, but behind every number is a person seeking help at their most vulnerable. The good news? Many of these errors are preventable. Here’s how:
- Strengthen communication with SBAR (Situation-Background-Assessment-Recommendation) tools and closed-loop confirmation.
- Use checklists and standardized protocols for triage, medication administration, and discharge.
- Promote a culture of transparency. Studies show that open apologies and error disclosure can reduce lawsuits while building trust.
- Address systemic stress and burnout with staffing solutions and mental health support.
- Invest in continued training and triage support technologies (like AI guidance) to help ensure accurate assessments.
Errors in the ER can be relentless, but they don’t have to be irreversible. Understanding the common emergency room errors, the roots of treatment errors, and how malpractice claims emerge helps both patients and providers stay safer. Sharing knowledge, advocating for clearer systems, and fostering compassion in crisis care can help transform high-pressure rooms into healing spaces.